Experiencing a headache after an injury can be more than just an annoying inconvenience. For many, it’s the beginning of a challenging journey known as Post-Traumatic Headache (PTH). This condition often arises unexpectedly and can linger long after the initial trauma. Understanding PTH is crucial for those affected, as well as their families and caregivers. By exploring its causes, symptoms, diagnosis, and treatment options, we can shed light on this complex issue and offer hope to those seeking relief from persistent pain. If you or someone you know has been struggling with headaches following an injury, keep reading—this guide is here to help!
Understanding Post-Traumatic Headache (PTH)
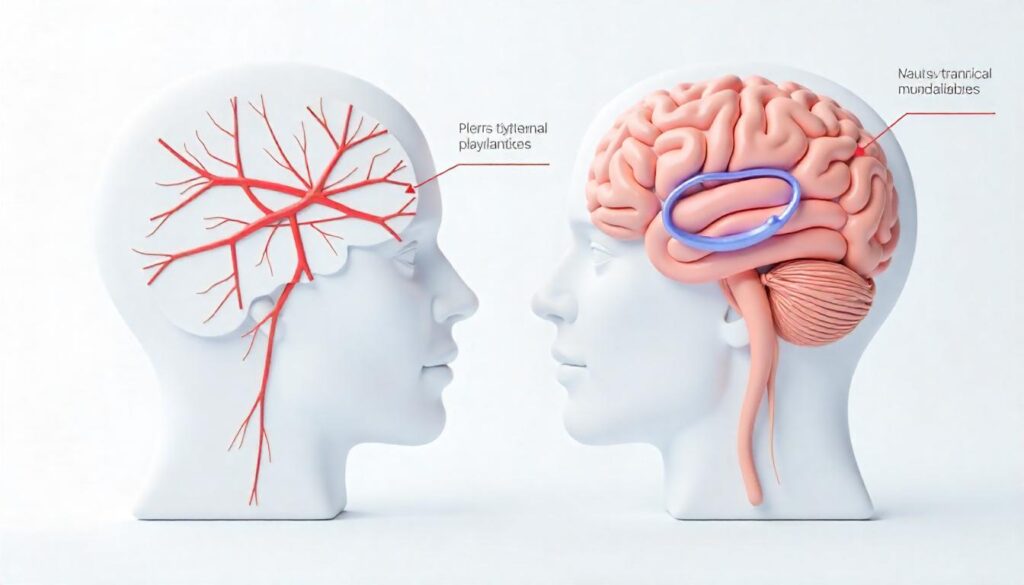
Post-Traumatic Headache (PTH) is a common condition that emerges after experiencing head or neck trauma. It’s not just an ordinary headache; it can significantly disrupt daily life and affect overall well-being.
This type of headache often occurs within days to weeks following the injury. While some people may recover quickly, others might face ongoing challenges that span months or even years.
PTH can manifest in various ways, making it essential for individuals to recognize its unique characteristics. Understanding this condition helps pave the way for effective management and treatment options tailored to individual needs.
The experience of PTH goes beyond physical pain—it can also impact emotional health. Many find themselves grappling with anxiety and frustration as they navigate their recovery journey. Recognizing these aspects is vital in addressing both the physical and psychological elements of PTH.
Causes of PTH
Post-traumatic headache (PTH) can arise from various factors. One major cause is head and neck injuries. Even minor trauma, like whiplash or a fall, may trigger persistent headaches.
Concussions or brain trauma are significant contributors to PTH as well. The impact on the brain can disrupt normal functioning and lead to chronic pain conditions.
Psychological factors also play a role in developing PTH. Stress, anxiety, or post-traumatic stress disorder (PTSD) can heighten sensitivity to pain and exacerbate symptoms following an injury.
Understanding these causes is crucial for effective management of post-traumatic headaches. Each case varies widely among individuals, making personalized treatment approaches essential for relief.
A. Head and neck injuries
Head and neck injuries are common culprits of post-traumatic headache (PTH). These injuries can occur from falls, sports accidents, or even car crashes. The impact may strain the muscles and ligaments in these areas.
When the head suddenly moves forward and backward—like during whiplash—the delicate structures of your neck can be affected. This tension often leads to persistent pain that spreads to the head.
Additionally, fractures or contusions in the skull can cause inflammation around the brain. As a result, headaches might develop days or weeks after an injury occurs.
Understanding how these physical traumas contribute to PTH is essential for effective treatment and management strategies moving forward. Keeping track of any discomfort following such incidents can help with early recognition of potential issues.
B. Concussions or brain trauma

Concussions and brain trauma are significant contributors to post-traumatic headaches. When the head experiences a sudden jolt or impact, it can disrupt normal brain function, leading to various symptoms.
During such an injury, the delicate tissues of the brain may stretch or tear. This disruption can trigger inflammation and chemical changes that result in persistent pain.
Individuals who have suffered concussions often report headaches that differ from their usual migraines or tension-type headaches. These pains may feel more intense and lingering.
Interestingly, some people might not immediately recognize a concussion’s effects. Symptoms can develop over hours or even days after the initial injury. Awareness of this delayed response is crucial for timely treatment.
Addressing these injuries early on may help alleviate headache symptoms later on. Effective management strategies can make a significant difference in recovery trajectories for those affected by concussions.
C. Psychological factors
Psychological factors can significantly contribute to the development of post-traumatic headache (PTH). After experiencing a traumatic event, individuals may face emotional challenges like anxiety and depression. These feelings can amplify physical symptoms, creating a feedback loop that intensifies pain.
Stress is another critical element. High levels of stress can trigger tension-type headaches, making PTH more likely. The mind-body connection plays an essential role here; mental strain often translates into physical discomfort.
Moreover, those with pre-existing psychological conditions might find their headaches worsening after trauma. It’s crucial to address these psychological aspects during treatment for PTH. Therapies that focus on mental well-being could prove beneficial in managing both the emotional and physical components of this condition. Recognizing the interplay between mind and body may pave the way for more effective interventions tailored to individual needs.
Symptoms of PTH
Post-Traumatic Headache (PTH) can manifest in various ways, making it crucial to recognize its symptoms early. One of the most common indicators is head pain and pressure that may feel different from a typical headache. This discomfort can range from mild to severe and often lingers for an extended period.
Many individuals with PTH also experience heightened sensitivity to light and sound. Everyday noises or bright lights that were once tolerable may suddenly become unbearable, contributing to an overall sense of unease.
Nausea and vomiting can accompany these headaches as well. The intense pain sometimes leads to digestive disturbances, adding another layer of challenge for those affected by PTH. Recognizing these symptoms is vital for seeking appropriate treatment options effectively.
A. Head pain and pressure
Head pain and pressure are hallmark signs of post-traumatic headache (PTH). This discomfort can manifest immediately after an injury or develop gradually over time. Many people describe it as a dull ache, while others may experience sharp, throbbing sensations.
The intensity of the pain can vary significantly. Some find it mild, barely registering in their daily activities, while others might struggle to concentrate or perform basic tasks due to debilitating pressure.
This type of headache often feels different from typical tension headaches. The location may change, shifting from one side of the head to another without warning. Sometimes it’s accompanied by a feeling of tightness around the temples.
Understanding this aspect is crucial for those experiencing PTH symptoms. Recognizing that head pain and pressure are part of this condition can help individuals seek appropriate care sooner rather than later.
B. Sensitivity to light and sound

Sensitivity to light and sound is a common symptom of post-traumatic headache. This heightened sensitivity, known as photophobia and phonophobia respectively, can significantly impact daily life.
Bright lights may feel glaring or overwhelming. Even soft lighting can become intolerable for those suffering from PTH. It’s not just about discomfort; it can lead to avoidance of social situations or outdoor activities altogether.
Similarly, loud noises are often unbearable. Conversations, music, or even everyday sounds like laughter might feel jarring. This reaction stems from the brain’s altered processing after an injury.
Living with these sensitivities requires adjustments in lifestyle. Many find solace in dimly lit rooms and quiet environments when experiencing these symptoms. Creating a calm space becomes essential for managing their well-being during flare-ups.
C. Nausea and vomiting
Nausea and vomiting can often accompany post-traumatic headache, adding to the distress of those affected. This symptom may arise shortly after an injury or develop over time.
The sensation of nausea is not merely uncomfortable; it can disrupt daily activities and impact quality of life. Many individuals describe a lingering queasiness that makes eating or drinking difficult.
Vomiting may occur sporadically, sometimes triggered by intense head pain or light exposure. These episodes can leave sufferers feeling weak and dehydrated.
Understanding this connection between headaches and gastrointestinal symptoms is essential for managing PTH effectively. Addressing both aspects offers a more comprehensive approach to relief.
Diagnosis of PTH
Diagnosing Post-Traumatic Headache (PTH) involves a comprehensive approach. The healthcare provider will start by reviewing your medical history. They’ll ask about any recent injuries, headaches, and existing conditions.
A thorough physical examination follows. This helps assess neurological function and identify any red flags in symptoms.
Imaging tests may be necessary for a clearer picture of the brain’s condition. A CT scan or MRI can reveal structural issues resulting from trauma.
It’s crucial to differentiate PTH from other headache disorders. Accurate diagnosis ensures appropriate treatment tailored to individual needs, alleviating discomfort effectively.
A. Medical history and physical exam
When diagnosing Post-Traumatic Headache (PTH), a thorough medical history is crucial. Your doctor will ask about any recent head or neck injuries, as well as your symptoms’ onset and duration. This information helps to pinpoint the cause.
A comprehensive physical exam follows. The physician checks for signs of neurological issues, like balance problems or cognitive difficulties. They may also assess your range of motion in the neck and head.
This examination isn’t just routine; it provides vital clues that can guide treatment decisions. By understanding your unique situation, healthcare professionals can tailor their approach effectively. Every detail matters when addressing PTH’s complexities in an individual case.
B. Imaging tests
Imaging tests play a crucial role in diagnosing Post-Traumatic Headache (PTH). These tests help healthcare professionals visualize the brain and neck structures, ruling out other potential issues.
Common imaging techniques include CT scans and MRIs. A CT scan provides detailed images of the brain, helping detect any bleeding or structural damage following an injury. This is particularly useful after concussions or trauma.
MRIs offer even more detail by capturing soft tissue images. They can reveal changes in the brain that may contribute to headache symptoms.
Doctors may recommend these procedures based on your history and physical examination findings. The results guide them toward appropriate treatment options tailored specifically for you.
Utilizing imaging tests ensures a comprehensive understanding of your condition, paving the way for effective management strategies aimed at alleviating PTH symptoms.
Treatment Options
When it comes to treating Post-Traumatic Headache (PTH), a comprehensive approach is often the most effective. The treatment plan typically depends on the severity of symptoms and their impact on daily life.
Medications are frequently used as a first-line defense. Over-the-counter pain relievers like ibuprofen or acetaminophen may provide relief for some individuals. For more severe headaches, prescription medications such as triptans or preventive treatments might be necessary.
Physical therapy can also play an essential role in recovery. It helps improve neck strength and flexibility, which can alleviate tension that contributes to headaches. Engaging in gentle exercises and stretches under professional guidance may lead to significant improvements over time.
Cognitive-behavioral therapy (CBT) has shown promise for those experiencing psychological factors related to PTH. Therapy sessions can equip individuals with coping strategies and stress management techniques, making it easier to deal with headache triggers.
Alternative therapies such as acupuncture or chiropractic care offer another layer of options for those seeking relief beyond traditional methods. These approaches have gained popularity due to their holistic nature and potential effectiveness without medication side effects.
Lifestyle modifications shouldn’t be overlooked either. Staying hydrated, maintaining a regular sleep schedule, avoiding known headache triggers—like specific foods or excessive screen time—and practicing relaxation techniques can contribute significantly to reducing headache frequency and intensity.
Each person’s journey with PTH is unique; therefore, tailoring treatment plans is crucial. Consulting healthcare professionals who specialize in post-traumatic conditions ensures you receive the best advice suited for your individual needs.
Understanding the various causes, recognizing symptoms early on, getting an accurate diagnosis, and exploring multiple treatment avenues all work together toward finding relief from post-traumatic headaches.
